Neural stem cell therapy combined with a common cold virus may be a highly effective way of improving outcomes in patients with newly diagnosed malignant gliomas.
Neural stem cell therapy combined with a common cold virus may be a highly effective way of improving outcomes in patients with newly diagnosed malignant gliomas.

Adult patients with early thymic precursor (ETP) acute lymphoblastic leukemia (ALL), a subgroup of T-cell ALL, could benefit from the use of response-based risk stratification and therapy intensification similar to that used in pediatric patients with ETP-ALL.

CTL019, an investigational chimeric antigen receptor T-cell therapy, demonstrated high response rates and a manageable safety profile in pediatric and young adult patients with relapsed and/or refractory acute lymphoblastic leukemia.
Results from the phase III Myeloma XI study showed that patients with myeloma had deeper responses after induction and after allo-stem cell transplantation with outpatient-delivered quadruplet therapy than with sequential immunomodulatory triplet combinations.

All patients with multiple myeloma in a phase I study showed a response following treatment with an active dose of bb2121, an investigational anti–BCMA CAR T-cell construct.

Investigators reported the characterization of early clinical and serum biomarkers that may identify specific patients with ALL being treated with 19-28z chimeric antigen receptor T cells needing an early intervention to mitigate the development of severe neurotoxicity.

No evidence of adverse events or significant safety concerns has surfaced.

Surgical resection, including cytoreductive nephrectomy, remains the standard of care for most patients with renal cell carcinoma, but many patients will have a recurrence, and could benefit from additional therapy.

Bijal D. Shah, MD, discusses the current treatment paradigm of MCL, what therapies are moving through the pipeline at a rapid rate, the potential benefit with CAR T-cell therapy, and pivotal biomarker studies currently being conducted.
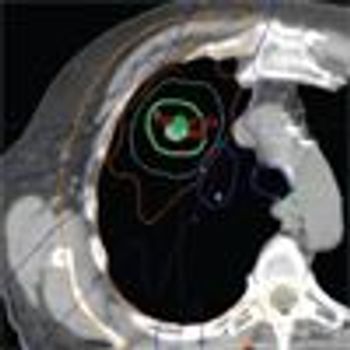
Three randomized trials of SBRT vs surgical resection closed due to poor accrual, but an analysis of patients treated in these trials suggested that SBRT might even be superior to surgery. New trials are underway to further assess the question of whether SBRT can be the definitive treatment for early-stage NSCLC instead of surgery.

Sarah Rutherford, MD, discusses rare DLBCL subtypes, ongoing research to improve outcomes for these patient populations, and the potential role of CAR T-cell therapy.

CAR T-cell therapy may have a role in combating relapsed/refractory multiple myeloma, according to new data from a phase I study presented at the 2017 ASCO Annual Meeting, held June 2–6 in Chicago.

Anti-CD19 CAR T-cell therapy may benefit patients with aggressive B-cell non-Hodgkin lymphoma who have relapsed or are refractory to standard therapy.

Epacadostat plus pembrolizumab yielded “encouraging response outcomes” among patients with 0 or 1 prior lines of therapy for advanced renal cell carcinoma.

Despite immune-related adverse events, concurrent ibrutinib and anti-CD19 CAR T-cell therapy may improve response rates in patients with chronic lymphocytic leukemia.

Analysis from a phase III trial confirmed the prognostic value of a 16-gene recurrence score in patients with high-risk renal cell carcinoma undergoing adjuvant sunitinib therapy.

Pazopanib 600 mg daily as adjuvant therapy did not prolong disease-free survival for patients with locally advanced renal cell carcinoma.

Concurrent treatment with CTL-119 cell therapy and ibrutinib (Imbruvica) led to complete marrow clearance of leukemic cells in 8 of 9 evaluable patients with heavily pretreated or genetically high-risk chronic lymphocytic leukemia, results of a pilot study showed.

The pharmacologic treatment for advanced renal cell carcinoma has evolved considerably since the FDA approved interleukin-2 as the first systemic therapy for the tumor type in 1992. Since then, the FDA has approved more than 20 drugs for RCC in the past 12 years.
A new gene therapy tested the efficacy of injecting a virus into the eye.

CAR T-cell therapy targeting B-cell maturation protein may be a new effective type of immunotherapy treatment for patients with multiple myeloma.
Early results from a Chinese study showed that 33 of 35 patients (94%) with relapsed or refractory multiple myeloma experienced clinical remission after treatment with chimeric antigen receptor T cells targeting B-cell maturation protein.

This review will focus on current therapies used in the first-line setting for advanced EGFR mutation positive non–small cell lung cancer (NSCLC) followed by emerging data that may lead to a transition in the choice for initial therapy in these patients.
The FDA has granted a priority review designation to sunitinib (Sutent) for use as an adjuvant therapy in patients with renal cell carcinoma who have received nephrectomy and are high risk for recurrence.

A new triple therapy approach using a checkpoint inhibitor and T-cell therapy is showing considerable promise in the treatment of Merkel cell carcinoma.

Based on the results of the phase 2 ZUMA-1 trial in patients with refractory non-Hodgkin lymphoma, Kite Pharma has submitted for, and received, a priority review for its chimeric antigen receptor (CAR)-T cell treatment, axicabtagene ciloleucel.

Higher doses of the kinase inhibitor brigatinib as second-line therapy for ALK-positive non–small-cell lung cancer may be an option for some patients.

More than one-third of patients with metastatic uveal melanoma had objective tumor regression when treated with adoptive transfer of autologous tumor-infiltrating lymphocytes.

This review will highlight the survival impact that rituximab therapy has had on major lymphoid malignancies, such as diffuse large B-cell lymphoma, chronic lymphocytic leukemia/small lymphocytic lymphoma, follicular lymphoma, and mantle cell lymphoma. We will also discuss alternative anti-CD20 monoclonal antibodies.

Researchers at Seattle Children's Research Institute announced the first-in-human clinical trial aimed to extend remission for children and young adults with leukemia treated with CAR T-cell immunotherapy.