Novartis’ just-approved chimeric antigen receptor (CAR) T-cell therapy tisagenlecleucel is going to be introduced on the market at a price of $475,000 for a single infusion, an amount that is within the range anticipated by oncologists.
Novartis’ just-approved chimeric antigen receptor (CAR) T-cell therapy tisagenlecleucel is going to be introduced on the market at a price of $475,000 for a single infusion, an amount that is within the range anticipated by oncologists.

The FDA issued a historic approval of the first chimeric antigen receptor (CAR) T-cell therapy, authorizing the use of tisagenlecleucel (Kymriah) for the treatment of patients up to 25 years of age with B-cell precursor acute lymphoblastic leukemia that is refractory or in second or later relapse.

The FDA has approved the first chimeric antigen receptor-T (CAR-T) treatment, tisagenlecleucel (Kymriah), for the treatment of B-cell precursor acute lymphoblastic leukemia in certain pediatric and young adult patients. The therapy represents a new frontier in cancer care.

Gilead Sciences will acquire Kite Pharma by the end of 2017 in an $11.9 billion transaction that will place Gilead at the forefront of chimeric antigen receptor-T (CAR-T) cell therapy development.

Despite all the excitement and anticipation, there is a growing anxiety among payers and providers regarding the cost of CAR T cells.

Chimeric antigen receptor (CAR)-T cells can re-expand in a lymphoma patient months after the initial infusion and can also be active against the patient’s cancer, according to a new study.

Shaji Kumar, MD, discusses his ixazomib maintenance trial, the latest FDA activity in myeloma, and the potential of chimeric antigen receptor (CAR) T-cell therapy in the field of myeloma.

Chimeric antigen receptor (CAR) T-cell therapies could spawn a new and lucrative industry in anticancer immunotherapy, resulting in single-infusion treatments costing hundreds of thousands of dollars, and even attracting medical tourism from abroad, where regulatory permissions are likely to come more slowly than in the United States.

Patients with newly diagnosed multiple myeloma treated with lenalidomide maintenance therapy after undergoing autologous stem-cell transplantation had significantly improved overall survival compared with observation or placebo.

Researchers have determined that CD30-specific CAR T cells could be used safely and induce durable complete responses in patients with Hodgkin lymphoma and anaplastic large cell lymphoma.
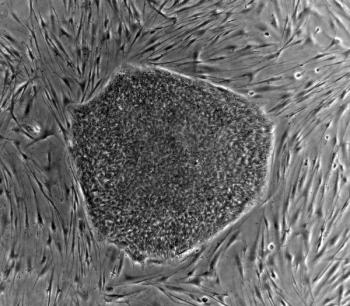
Companies are skirting regulation to be the first to build the next big stem cell therapy, creating clinical concerns and poor patient outcomes.

The Institute for Clinical and Economic Review (ICER) has released a draft version of their scoping document that will compare the clinical effectiveness and value of 2 chimeric antigen receptor (CAR)-T cell treatments being reviewed by the FDA.

A biomarker for pancreatic precursor cells might give researchers a shortcut to create insulin-producing beta cells that can be transplanted into patients with type 1 diabetes.

Surgical management of the patient with non–small-cell lung cancer (NSCLC) is complex. When should stereotactic body radiation therapy be used? What are the advantages of video-assisted thoracic surgery? Test your knowledge in our latest quiz.

There’s a lot happening in clinical practice with immunotherapy treatments: expanded indications for nivolumab and ipilimumab, biomarkers to judge patient response to combinations, and developments with CAR-T.

Acalabrutinib has been granted FDA Breakthrough Therapy Designation for the treatment of patients with mantle cell lymphoma who have relapsed or have received at least one prior therapy.

The new immunotherapy of chimeric antigen receptor (CAR)-T cells has demonstrated the ability to increase clinical remission in multiple myeloma patients by targeting the B-cell maturation protein that participates in disease progression.

The FDA has granted acalabrutinib a breakthrough therapy designation for patients with previously-treated mantle cell lymphoma.

Saad Z. Usmani, MD, discusses recent multiple myeloma data, the potential role of CAR T-cell therapy, and what therapeutic advancements the community can expect in the remainder of 2017.

Treatment with CD19 chimeric antigen receptor-modified T-cell therapy induced a high response rate in patients with high-risk, ibrutinib-refractory chronic lymphocytic leukemia.

Sattva S. Neelapu, MD, discusses the latest results for axicabtagene ciloleucel (KTE-C19) for transplant-ineligible patients with relapsed/refractory non-Hodgkin lymphoma and the CAR T-cell therapy’s potential to be a new standard of care.

A study on long-term remission of diffuse large B-cell lymphoma (DLBCL) shows that Kite Pharma’s anti-CD19 chimeric antigen receptor-T (CAR-T) cell treatment resulted in remission for up to 56 months.

The Sanford Project: T-Rex Study has reached its midway point through a Phase II, fast-tracked trial.

Ezra Cohen, MD, discusses anti–PD-1/PD-L1 combination regimens in HNSCC, the potential for CAR T-cell therapy, and remaining challenges with immunotherapy in the field.

ARCHER 1050, the first phase 3 head-to-head study of epithelial growth factor receptor (EGFR) tyrosine kinase inhibition, has produced results that demonstrate statistically significant and clinically meaningful improvement with dacomitinib compared with gefitinib (Iressa) as first-line therapy for non—small cell lung cancer (NSCLC) with EGFR-activating mutations.

If approved, LUXTURNA would also be the first pharmacological treatment for inherited retinal disease

ODAC approval of Novartis' CAR T-Cell therapy paves the way for its FDA approval as a commercially available treatment for B-cell ALL.

Bajil J. Shah, MD, discusses the significant impact CAR T-cell therapy can have on the treatment landscape for patients with acute lymphoblastic leukemia.

CTL019 was unanimously approved by FDA’s Oncologic Drugs Advisory Committee (ODAC) for the treatment of children and young adults with relapsed or refractory B-cell acute lymphoblastic leukemia.

Novartis’ chimeric antigen receptor T-cell (CAR-T) therapy for treating pediatric leukemia is on the cusp of being the first FDA-approved gene therapy, which will lead to new developments and utilizations of CAR-T therapy for treating other advanced blood cancers.