
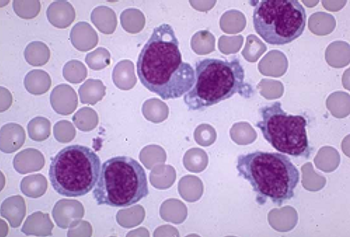
A blood test that tracks the rise and fall of circulating tumor DNA (ctDNA) levels can predict how patients with diffuse large B-cell lymphoma will respond to therapy within days of starting treatment.

A blood test that tracks the rise and fall of circulating tumor DNA (ctDNA) levels can predict how patients with diffuse large B-cell lymphoma will respond to therapy within days of starting treatment.

Axicabtagene ciloleucel (axi-cel; Yescarta) is being evaluated in patients with relapsed or refractory mantle cell lymphoma—a rare B-cell non-Hodgkin lymphoma that contributes 4200 new patients in the United States each year.

The designation is backed by positive interim data from ASPIRO, which has demonstrated significant improvements in neuromuscular and respiratory function at week 24.
The first chimeric antigen receptor (CAR) T-cell therapy was approved just a year ago, changing the face of treatment for certain types of leukemias and lymphomas but carrying with it the downsides of toxicity and cost. A year later, scientists from a major cancer center said that they’ve made headway to discovering more about the T-cell signaling patterns and that understanding more about the biological pathways could help design the next generation of CAR-T treatments.

The FDA has granted a fast track designation to gene therapy product candidate AAV-CNGB3 for the treatment of achromatopsia caused by mutations in the CNGB3 gene.

The FDA has approved Bristol-Meyers Squibb Company’s nivolumab (Opdivo) for the treatment of metastatic small cell lung cancer (SCLC) that has progressed after platinum-based chemotherapy and at least 1 other line of therapy.

The FDA has approved single-agent nivolumab for the treatment of patients with small cell lung cancer with disease progression following 2 or more lines of therapy.

Next week, a CMS committee will hold a day-long meeting to discuss a national coverage determination (NCD) for chimeric antigen receptor (CAR) T-cell immunotherapies, and in Thursday’s New England Journal of Medicine, Peter B. Bach, MD, MAPP, reviewed several strategies open to CMS as it continues to try to determine how to pay for CAR T.

The FDA will start to review gene therapy experiments and products the same as other treatments and drugs; Alaska and Minnesota have become models for other states looking to curb health insurance premium increases with reinsurance programs; patients with limited English proficiency often have to rely on family members and friends to interpret for them, which can have serious consequences.
In an effort to reprogram retina cell regeneration, investigators activated dormant stem cells then aided other stem cells in developing into rod photoreceptor cells—the most abundant cell type in the retina which first aid the retina in sensing light.

The STRIvE-01 study explored the safety of CAR T-cell therapy in children and young adults with relapsed or refractory solid tumors.

Andre Goy, MD, shares insight on the new array of treatment options for mantle cell lymphoma and how to properly implement them.

Ian W. Flinn, MD, PhD, discusses the latest developments with CAR T-cell therapies and other recent advances in the field of lymphoma.
Researchers from the University of Texas MD Anderson Cancer Center, along with the Pediatric Acute Lung Injury and Sepsis Investigators Network (PALISI), recently published guidelines in Nature Reviews Clinical Oncology for the management of chimeric antigen receptor (CAR) T-cell therapy for children with acute lymphoblastic leukemia.

The FDA has approved mogamulizumab for the treatment of patients with cutaneous T-cell lymphoma who have received at least 1 prior systemic therapy.

The REGENXBIO drug's promising phase 1 results has led to the addition of a fourth patient dosing cohort and a phase 2 trial initiation.

Celyad, a biopharmaceutical company that focuses on the development of chimeric antigen receptor (CAR) T-cell therapies, recently announced that the FDA has accepted its Investigational New Drug (IND) application for CYAD-101, the first non–gene-edited allogeneic clinical program.

CMS announced a raft of final rulemaking Thursday for 2019, including ending the so-called 25% rule for long-term care hospitals, and approving add-on payments estimated to cost about $72 million for chimeric antigen receptor (CAR) T-cell immunotherapy.

Tumor-treating field therapy, which uses low-intensity electrical fields to disrupt cancer cell division and promote cell death, has gained a frontline approval in glioblastoma. Several pivotal clinical trials have been launched to determine whether the technology can help patients with other solid tumors.
A murine study suggests this engineered combination may offer a major advantage over current CAR T-cell–based immunotherapies.

As the checkpoint inhibitors move into the frontline setting for patients with non–small cell lung cancer, the focus has been placed on the duration of therapy and what to do in the second-line setting following progression.

How the three-year results of a gene therapy for inherited retinal disease may redefine its potential in ophthalmology.

CAR T-Cell therapy updates presented at the American Society of Clinical Oncology's Annual Meeting held June 2018.

A third-party manufacturing issue has delayed a phase I/IIa study for Sarepta Therapeutics.

New research highlights the potential of fetal gene therapy to prevent and cure neonatal lethal neurodegenerative diseases in humans in utero.

A three-year update of VN for patients with biallelic RPE65 mutation-associated inherited retinal disease improved on the common standard-of-care for retina disease.

A review of available evidence has led the American Society for Radiation Oncology to issue a strong recommendation for use of concurrent chemotherapy with thoracic external beam radiation therapy in a subset of patients with incurable stage III non–small cell lung cancer.
The FDA approved the first targeted therapy for adults with relapsed or refractory acute myeloid leukemia with an IDH1 mutation. In addition, FDA also approved a companion diagnostic to be used to detect the specific mutations in the IDH1 gene.

Though cell therapies have gained FDA approval to treat any ocular disease, companies have marketed predominately to patients with AMD, with procedures that could lead to blindness.

New findings suggest that a specific hemoglobin production protein could be a target for therapy in sickle cell disease or beta-thalassemia.